Types of gum disease
There are many forms and stages of periodontal disease. The most common are:
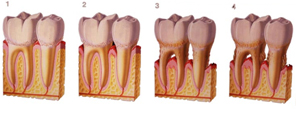
1. Gingivitis. The first stage of periodontal disease, gingivitis, is the mild inflammation of the gingival caused by plaque build up. Gingivitis is an inflammatory condition of the gingiva caused by factors including smoking, certain drugs and hormonal changes that occur in puberty and pregnancy. Your gingival will be red, swollen, and tender. You may also notice bleeding while you brush and floss. This stage of gingivitis is reversible.
2. Mild Periodontitis. Inflammation will spread to the supporting alveolar bone. Minor bone loss and the formation of periodontal pockets, or food traps, may occur. Periodontitis follows with the destruction of the supporting structure of the teeth and is influenced by factors including the individual's immune and inflammatory response. It is initiated by microbial plaque. Periodontitis, if left untreated, can causes tooth loss, mouth odor, bad breath or halitosis.
3. Moderate Periodontitis. In this stage, there will be increased gingival recession, moderate to deep pockets, moderate to severe bone loss, and mobility of teeth due to the bone loss.
4. Severe Periodontitis. This is the most serious stage of periodontitis. Deep pockets, increased mobility of teeth, movement of teeth out of position, and visible fistulas (boils) will be present in this stage. Pus may develop; bone loss continues, and your teeth may loosen or fall out.
How is Periodontal (Gum) Disease Treated?
In the event you are diagnosed with gum disease, your gum dentist / periodontist may recommend non-surgical periodontal treatment. For advanced cases, gum surgery may be required. The biggest factor in the treatment options available to you will be how quickly your gum disease is detected and how rapidly it advances.
Treatment will depend upon the type of periodontal disease and how far the condition has progressed.
1. Non-Surgical Treatment. It will be applied if the patient is still in the early stages of
2. Scaling or Cleaning. It is a treatment procedure which involves the instrumentation of the crown and root surfaces of the teeth. Plaque, calculus, and stains will be removed from these surfaces. It is performed on patients with periodontal disease and is therapeutic, as apposed to prophylactic and may precede root planning. It is a definitive, meticulous treatment procedure aimed at the removal of cementum and/or dentin that is rough and is possibly permeated by calculus, or even contaminated with toxins or microorganisms. This procedure can be used as a definitive treatment or as part of pre-surgical therapy ("tissue preparation") depending on how far the periodontal disease has advanced.
3. Bone or Gingival Augmentation. This is a surgical procedure which uses a barrier membrane and or bone graft replacement material placed under the gum and over the remaining bone support (ridge or jaw bone) to aid the regeneration of new bone in an area where teeth are being extracted or have already been removed. The graft material may be taken from the patient's own body. If not, an artificial, synthetic, or natural substitute may be used. This prevents the surrounding bone from collapsing into the extraction socket after the removal of a tooth. If this procedure is not carried out, the ridge will become narrow and sharp and it will not be possible to insert an implant or a comfortable-fitting denture.
4. Post-Op care. In most cases, the gums are too tender to brush post-operatively. We will provide you with an antibacterial mouth rinse called chlorhexidine which will chemically reach those areas that the tooth brush will be too sensitive to debride. Warm salt water will help to reduce gum inflammation and an antibiotic is usually prescribed to prevent infection. Analgesics (pain medication) can be used if the pain becomes severe.

